- Manoj Sivan, associate clinical professor and honorary consultant in rehabilitation medicine1,
- Shaney Wright, long covid patient and advocate,
- Sarah Hughes, research fellow2, honorary research fellow3,
- Melanie Calvert, professor of outcomes methodology4
- 1University of Leeds, Leeds Teaching Hospitals NHS Trust and Leeds Community Healthcare NHS long covid service
- 2Centre for Patient Reported Outcome Research, University of Birmingham
- 3Faculty of Medicine, Health, and Life Science; Swansea University
- 4University of Birmingham
Management expert Peter Drucker’s famous words “if you can’t measure it, you can’t manage it” holds good for post-covid syndrome, or long covid, which affects an estimated two million individuals in the UK 1 and extrapolated prevalence data suggests more than 50 million individuals may be affected worldwide.2 Long covid is a multisystem condition with over 200 symptoms reported across most of the organ systems, often with a chronic fluctuating pattern of presentation.3 With up to 30% of covid-19 health burden being related to covid induced disability, long covid presents substantial challenges for healthcare systems worldwide.4 Management of this complex syndrome, in part, requires new integrated long covid services with expertise drawn from a range of specialists across disciplines from both primary and secondary care.56 Healthcare services globally are investing in these new pathways of care, but there are no agreed measurement metrics yet to comprehensively capture patient experience or the effectiveness of treatments, partly due to lack of clear biomarkers for the condition.
Patient reported outcome measures (PROMs) are questionnaire tools to ascertain patients’ views of their symptoms, their functional status, and their health-related quality of life.7 PROM use in other routine clinical contexts have been shown to facilitate communication, engage patients in their care, tailor care to individual patients’ needs, and show value for money for those investing in the services.89 Clinical outcome assessments should include clinically important concepts that define the disease in the target population, assess the impact of disease, and reflect the lived experience of those with the condition. Given the large scale, relative novelty, and multifariousness of long covid syndrome, coupled with shortcomings in understanding viral-onset illness, it is unsurprising that standardised assessments of functioning, disability, and health are lacking.1011
Currently long covid services are using PROMs developed for other conditions such respiratory conditions (Medical Research Council Dyspnea Scale), anxiety disorder (Generalised Anxiety Disorder Assessment) and depression (Patient Health Questionnaire) and a range of other symptom-specific PROMs that have not yet been validated for use with long covid.121314 However, this approach has several limitations. Such measures, in our experience, are cognitively burdensome to long covid patients, do not comprehensively capture the spectrum of symptoms, cannot directly engage with the underlying biological mechanisms, and are reported not to be meaningful by patients, families, and clinicians. Using a range of symptom specific measures makes it challenging to repeat the measures frequently to capture day by day fluctuations and are difficult to implement in busy services overburdened with managing such a large caseload of patients. There is the added danger of misleading management, for example individuals scoring highly on anxiety scores may get diverted to psychological services when their anxiety is being driven by underlying dysautonomia (increased heart rate) which needs medical optimisation.
Clinicians, services, and researchers need to invest their energies in developing and validating long covid specific PROMs or validating existing PROMs for use in long covid routine clinical practice and research settings for long covid. Condition specific PROMs can provide valuable information on symptom range, severity, functional impact—and more importantly—in combination with biomedical research, help understand underlying mechanisms, phenotypes, and traits in this heterogeneous clinical syndrome.11 Such measures can be used to support individuals with self-management and monitoring, in addition to supporting healthcare services to align long covid care with health system goals. The PROMs need to measure not only symptom range, but also burden in daily activities, including impact on family life, leisure, and work. The World Health Organisation (WHO) provides a very useful framework of International Classification of Functioning Disability and Health (ICF) to understand the various aspects of any health condition and its interaction with the affected individual which could be conceptualised in selecting measures to understand long covid in its totality.15
Patient groups—including under-served populations—need to be involved in the development, selection, and co-design of systems to implement long covid specific PROMs in care pathways.8 There needs to be early engagement with other key stakeholders—clinicians, health informatics, governance, researchers, and service commissioners. When using a combination of measures, we need to develop a least burdensome set of PROMs that can be used across clinical and research settings and applicable to low, middle-, and high-income countries. PROMs should empower patients to self-monitor their condition and help them understand the physical, cognitive, and emotional triggers of their condition.16 Healthcare services should also be able to use these PROMs to evaluate their investment and effectiveness of the care being delivered. Through careful selection and robust, well planned implementation, PROMs, as part of a combination of initiatives, have potential to enhance the care of the millions of people living with long covid.
Footnotes
References
- ↵
- WhitakerM
- ↵
- HirschtickJL,
- TitusAR,
- SlocumE,
- et al
OpenUrlCrossRefPubMed - ↵
- BrownDA,
- O’BrienKK
OpenUrlFREE Full Text - ↵
- BriggsA,
- VassallA
OpenUrlCrossRefPubMed - ↵NHSEngland. National guidance for post-COVID syndrome assessment clinics. 2021.
- ↵
- SivanM,
- RaynerC,
- DelaneyB
OpenUrlFREE Full Text - ↵
- BlackN
OpenUrlAbstract/FREE Full Text - ↵
- SnyderCF,
- AaronsonNK,
- ChoucairAK,
- et al
OpenUrlCrossRefPubMedWeb of Science - ↵
- CalvertM,
- KyteD,
- PriceG,
- ValderasJM,
- HjollundNH
OpenUrlFREE Full Text - ↵
- O’ConnorRJ,
- PrestonN,
- ParkinA,
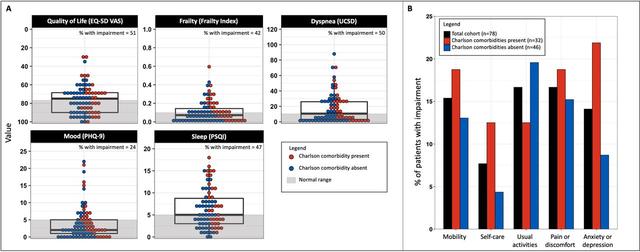
- et al
OpenUrlCrossRefPubMed - ↵
- SivanM,
- ParkinA,
- MakowerS,
- GreenwoodDC
OpenUrlCrossRefPubMed - ↵
- HeightmanM,
- PrasharJ,
- HillmanTE,
- et al
OpenUrlAbstract/FREE Full Text - ↵
- EvansRA,
- McAuleyH,
- HarrisonEM,
- et al.,
- PHOSP-COVID Collaborative Group
OpenUrlCrossRefPubMed - ↵
- ParkinA,
- DavisonJ,
- TarrantR,
- et al
OpenUrlCrossRefPubMed - ↵
- PatelK,
- StraudiS,
- Yee SienN,
- FayedN,
- MelvinJL,
- SivanM
OpenUrlCrossRefPubMed - ↵WHO. Support for rehabilitation: self-management after COVID-19-related illness. Copenhagen: WHO Regional Office for Europe; 2021. Available from: https://apps.who.int/iris/handle/10665/344472.